Obesity & COVID Long Haul: The Hidden Connection. In the labyrinth of health concerns that shadow our modern world, obesity and COVID-19 stand as twin colossi, casting long, intertwined shadows across the global landscape. The prevalence of obesity, a condition not merely of excess weight but of heightened health risks, has burgeoned into a pandemic in its own right, long before the coronavirus commandeered the world’s attention. Meanwhile, COVID-19, a novel adversary, has unfurled a tapestry of symptoms and sequelae, among which ‘long COVID’ looms ominously, a specter of prolonged suffering.
Yet, beneath the surface of these health crises lies a nexus seldom explored with the depth it demands—the intricate interplay between obesity and COVID-19, particularly in the context of long-haul symptoms. This intersection is not merely a confluence of conditions; it is a crucible in which the complexities of human health are both revealed and tested.
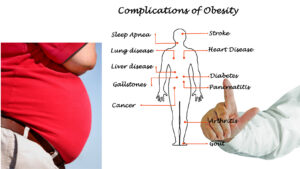
The dialogue surrounding obesity often orbits around well-trodden themes: the risks of cardiovascular disease, diabetes, and a slew of other chronic conditions. Similarly, discussions about COVID-19 tend to focus on its acute manifestations and the global race for containment and vaccination. However, the nuanced relationship between obesity and the long-term repercussions of COVID-19—affectionately termed ‘long COVID’—is a path less trodden, a narrative less told.
This article seeks to illuminate this shadowed path, to explore the subtleties and intricacies of how obesity intertwines with the long-term effects of COVID-19. It is a journey into the heart of a complex medical enigma, one that affects a significant swath of our global populace. From the immunological underpinnings to the clinical manifestations, we will delve into the evidence that paints a picture of this connection, all while maintaining a lens of objectivity and scientific rigor.
As we embark on this exploration, it is crucial to acknowledge that this is not a journey of fear-mongering or stigmatization. Obesity is not a choice, but a multifaceted health condition influenced by a constellation of genetic, environmental, and societal factors. Similarly, long COVID is not a sign of weakness, but a legitimate and often debilitating medical phenomenon. Our exploration is one of understanding, of compassion, and of a relentless pursuit of knowledge in the service of those who suffer in silence.
Understanding Obesity
In the tapestry of modern health discourse, obesity is often painted with broad, impersonal strokes—a condition defined by numbers on a scale and body mass index (BMI) charts. Yet, to truly understand obesity is to recognize it as a deeply personal, multifaceted phenomenon, one that transcends the simplicity of excess weight and ventures into the complex interplay of biology, environment, and psychology.
At its core, obesity is a state of energy imbalance over a prolonged period, where caloric intake surpasses energy expenditure. However, this clinical definition scarcely scratches the surface of its true nature. Obesity is not merely a physical condition; it is a silent storyteller of our times, narrating tales of societal shifts, technological advancements, and cultural transformations. It speaks of the ubiquity of processed foods, the sedentary shackles of modern occupations, and the intricate genetic tapestries that predispose some to store energy more readily than others.
The global impact of obesity is a mosaic of paradoxes. It is both a product of abundance and a harbinger of scarcity—scarcity of health, vitality, and, often, social acceptance. In a world where food deserts coexist with fast-food abundance, obesity has emerged as a democratic affliction, sparing neither the affluent nor the impoverished. Its prevalence is a reflection not only of individual choices but of the collective ethos of societies and the policies that shape them.
Yet, amidst this narrative, a seldom-discussed truth lingers: obesity is not an equal-opportunity condition. It is intricately woven with the threads of socioeconomic status, education, and access to healthcare. It is both a cause and a consequence of health disparities, a condition that can both stem from and exacerbate social inequities. The zip code can often predict the likelihood of obesity more accurately than genetic code, a testament to the profound influence of environment and access on health.
In understanding obesity, it is crucial to dismantle the stigma that often accompanies it. Obesity is not a character flaw or a moral failing; it is a complex chronic condition that requires empathy, understanding, and comprehensive management. It is a condition that can touch the lives of anyone, regardless of age, gender, or socioeconomic status, and one that demands a nuanced, compassionate approach in both discourse and care.
COVID-19: A Brief Overview
COVID-19, a term that once held no meaning in our collective lexicon, has rapidly evolved into a household name, synonymous with uncertainty, upheaval, and a global health crisis of unprecedented scale. Caused by the novel coronavirus SARS-CoV-2, COVID-19 has not only challenged our healthcare systems but has also forced a profound introspection into the very fabric of our societies.
The virus, with its crown-like spikes, has proven to be an insidious adversary, capable of both overt devastation and silent transmission. Its symptoms, ranging from mild coughs to severe respiratory distress, have painted a picture of a disease that is as unpredictable as it is pervasive. Yet, beyond the acute symptoms lies a shadow pandemic, a constellation of prolonged effects known as ‘long COVID,’ which continues to baffle and burden even the most resilient of survivors.
Long COVID, or post-acute sequelae of SARS-CoV-2 infection (PASC), is a term that encapsulates the lingering aftermath of the virus. It is a syndrome characterized by a spectrum of symptoms that persist long after the acute phase of the infection has subsided. From debilitating fatigue to persistent brain fog, long COVID has emerged as a chameleon of conditions, manifesting differently in each individual it touches.
The narrative of COVID-19 is often dominated by statistics—cases, deaths, vaccination rates. Yet, what is seldom discussed is the silent toll it takes on the ‘invisible’ victims, those grappling with long COVID in the quiet corners of post-infection life. These individuals navigate a labyrinth of symptoms, often without the compass of medical understanding or the visibility of acute sufferers.
As we delve into the intricacies of COVID-19, it is imperative to approach the subject with a lens that captures not only the clinical aspects but also the human stories behind the numbers. It is a tale of resilience and vulnerability, of science and uncertainty, and of a world grappling with an invisible enemy that has left indelible marks on the canvas of human health.
Exploring the Link: Obesity and COVID-19
As the world grapples with the multifaceted challenges posed by COVID-19, a pattern has emerged, weaving a complex tapestry that links obesity with more severe outcomes of the virus. This connection, though initially observed anecdotally, has since been substantiated by a growing body of research, painting a picture of obesity not just as a global health concern, but as a significant risk factor in the battle against COVID-19.
A pivotal study, published in the esteemed Lancet Diabetes & Endocrinology journal, sheds light on this intricate interplay. The research delves into the epidemiological data, drawing a correlation between higher body mass index (BMI) and an increased risk of severe outcomes from COVID-19, including hospitalization, admission to intensive care units, and even mortality. This study is not an isolated narrative but part of a chorus of scientific voices that echo a similar message: obesity amplifies the threat posed by COVID-19.
The link between obesity and COVID-19 severity can be attributed to several factors, each intertwining in a complex dance of pathophysiology. Firstly, obesity is often accompanied by a state of chronic, low-grade inflammation. This inflammatory milieu can prime the body for a more robust and potentially detrimental immune response to the virus, a phenomenon known as a cytokine storm. This hyperactive immune response can lead to widespread tissue damage, multi-organ failure, and, in severe cases, death.
Secondly, obesity is associated with alterations in respiratory physiology. Excess adipose tissue, particularly around the abdomen, can impede lung expansion, reducing functional residual capacity and impairing gas exchange. This mechanical disadvantage can exacerbate the respiratory distress that is a hallmark of severe COVID-19, making it more challenging to manage and recover from the infection.
Moreover, obesity is often a comorbid condition, existing alongside other health issues such as hypertension, diabetes, and cardiovascular disease. These comorbidities, in themselves risk factors for severe COVID-19, create a compounded risk profile that can make managing and treating the virus more complex and less predictable.
The relationship between obesity and COVID-19 is also a reflection of broader societal and health inequities. Obesity prevalence is disproportionately higher in socioeconomically disadvantaged populations, the same groups that have been hit hardest by the pandemic. These populations often face barriers to healthcare access, live in higher-density areas where the virus spreads more readily, and are more likely to be employed in essential services where remote work is not an option. Thus, the link between obesity and COVID-19 is not merely a matter of individual health but a mirror reflecting the systemic disparities that pervade our societies.
In exploring the link between obesity and COVID-19, it is crucial to approach the subject with nuance and empathy. Obesity is not a choice, but a complex condition influenced by a myriad of factors beyond individual control. The heightened risk it poses in the context of COVID-19 is not a cause for stigma but a call to action—a reminder of the urgent need for comprehensive public health strategies that address both the pandemic and the obesity epidemic with equal vigor and compassion.
Delving Deeper: Obesity and COVID Long Haul
The narrative of COVID-19 is incomplete without addressing the enigmatic phenomenon of long COVID, a condition characterized by a constellation of lingering symptoms that persist well beyond the acute phase of the infection. As we delve deeper into the labyrinth of COVID-19’s long-term effects, the spotlight turns to a particularly vulnerable group: individuals with obesity. The link between obesity and long COVID is not merely a correlation but a window into the intricate ways in which obesity can influence the trajectory of viral diseases.
A comprehensive study published in the International Journal of Obesity provides valuable insights into this connection. The research highlights that individuals with obesity are not only at a higher risk of developing severe COVID-19 but are also more susceptible to experiencing prolonged symptoms, a condition now widely recognized as long COVID. This susceptibility is not a mere coincidence but a reflection of the complex interplay between obesity, immune function, and viral pathogenesis.
One of the key mechanisms underlying this link is the state of chronic inflammation associated with obesity. Adipose tissue, particularly in excess, functions not just as a storage depot for energy but also as an active endocrine organ, secreting a variety of cytokines and inflammatory mediators. This chronic inflammatory state can disrupt immune homeostasis, leading to a dysregulated response to viral infections. In the context of COVID-19, this dysregulation can manifest as a prolonged and aberrant immune response, contributing to the persistence of symptoms that characterize long COVID.
Furthermore, obesity is known to impact vascular health, contributing to endothelial dysfunction and a pro-thrombotic state. COVID-19, in turn, has been shown to have a significant impact on the vascular system, causing endothelial injury and microvascular thrombosis. The convergence of these two factors can exacerbate the vascular complications of COVID-19, potentially prolonging recovery and contributing to the persistence of symptoms such as fatigue, dyspnea, and cognitive impairment.
The study also sheds light on the metabolic implications of obesity in the context of long COVID. Obesity is often accompanied by metabolic dysregulation, including insulin resistance and altered lipid metabolism. These metabolic disturbances can influence the body’s ability to mount an effective antiviral response and may impair the recovery process, leading to a protracted course of illness.
It is also important to consider the psychosocial dimensions of obesity in the context of long COVID. The stigma and discrimination associated with obesity can lead to increased psychological stress, which can, in turn, impact immune function and disease progression. Additionally, individuals with obesity may face barriers to accessing healthcare and support services, further complicating their recovery journey.
In delving deeper into the link between obesity and COVID long haul, it becomes evident that the relationship is multifactorial, involving a complex interplay of immunological, metabolic, vascular, and psychosocial factors. This understanding underscores the need for a holistic approach to managing long COVID in individuals with obesity, one that addresses not only the physical but also the emotional and social dimensions of their health. It is a call to action for healthcare providers, policymakers, and society at large to recognize the unique challenges faced by individuals with obesity in the era of COVID-19 and to work collaboratively towards solutions that are inclusive, empathetic, and grounded in scientific understanding.
Addressing the Issue
In the shadow of the COVID-19 pandemic, the link between obesity and long COVID presents not just a challenge but an opportunity—an opportunity to address a pervasive health issue with renewed vigor and a holistic approach. For health-conscious individuals aged 25 to 60, understanding the intersection of obesity and long COVID is the first step toward empowerment. Here are actionable strategies to address the issue:
-
Lifestyle Modifications:
– Nutritional Interventions: Adopt a balanced diet rich in whole foods, lean proteins, and vegetables while minimizing processed foods and sugars. Nutrition plays a pivotal role in managing weight and bolstering immune function.
– Physical Activity: Incorporate regular physical activity into your routine. Even moderate exercise can have profound effects on weight management and overall health.
– Stress Management: Chronic stress can contribute to weight gain and weaken the immune system. Practices like mindfulness, yoga, or even simple breathing exercises can mitigate stress.
-
Medical Interventions:
– Professional Guidance: Consult healthcare professionals for personalized advice. A tailored plan can address individual health needs more effectively.
– Weight Management Programs: Consider structured weight management programs that offer support and accountability.
– Medication and Surgery: In some cases, medication or bariatric surgery may be appropriate. These options should be discussed with a healthcare provider.
- Community and Policy Initiatives:
– Advocacy for Healthier Environments: Advocate for policies that promote healthier food options and physical activity in communities.
– Access to Healthcare: Support initiatives that improve access to healthcare for all, particularly for preventive services related to obesity and COVID-19.
- Education and Awareness:
– Informative Campaigns: Participate in or support campaigns that raise awareness about the link between obesity and long COVID.
– Sharing Personal Stories: Sharing experiences can be powerful. If comfortable, discuss your journey with others to inspire and educate.
Addressing the issue of obesity in the context of long COVID requires a multifaceted approach that encompasses lifestyle changes, medical interventions, community support, and policy initiatives. It’s about creating an environment that not only fosters individual health but also cultivates a society resilient to the challenges posed by pandemics like COVID-19. As we navigate this path, it’s crucial to remember that every step taken towards better health is a victory, not just for the individual, but for the community at large.
Conclusion
As we draw the curtains on our exploration of the intricate nexus between obesity and COVID-19, particularly its long-haul effects, we are left with a tapestry rich in complexity and nuance. This journey has taken us through the labyrinthine pathways of immunology, the societal underpinnings of health, and the deeply personal struggles that accompany both obesity and long COVID. It is a narrative that transcends the boundaries of individual health, touching upon the very essence of our collective human experience in the face of a global pandemic.
In this discourse, we have unearthed truths that are seldom whispered in the corridors of mainstream health dialogues. We have recognized obesity not as a standalone condition, but as a multifaceted phenomenon interwoven with the fabric of society, culture, and individual biology. We have seen how it casts a long shadow over the COVID-19 landscape, influencing not just the acute phase of the infection but the prolonged battle that many face in its aftermath.
The link between obesity and long COVID is a clarion call for a paradigm shift in how we approach health and disease. It is a reminder that health is not a commodity to be taken for granted but a mosaic of factors that require a holistic and empathetic approach. It beckons us to look beyond the numbers on a scale or the clinical definitions of a virus, urging us to see the human stories, the struggles, and the resilience that define our collective journey through this pandemic.
As we move forward, let this exploration serve as a beacon, illuminating the path towards a more inclusive, compassionate, and comprehensive approach to health. Let it remind us that in the face of adversity, our greatest strength lies in our ability to understand, adapt, and support one another. The link between obesity and long COVID is not just a medical phenomenon; it is a testament to the interconnectedness of our health, our societies, and our shared humanity.